YourPath Data Point: Co-occurring disorders
We collect an incredible amount of data here at YourPath, and with the help of Yunyang Zhong, a student at Macalester University, we have been able to analyze our data at a level that was previously impossible.
As we continue to leverage our data collection and analysis efforts to improve care not only in our corner of the system — but across populations at large — it will be vital to identify data points which might help to drive systemic improvements. We will be posting periodically about singular data points and what we might learn from them.
co-occurring disorders
Most individuals diagnosed with a substance use disorder (SUD) are also diagnosed with a mental health disorder. Numerous national population studies have shown that roughly half of those who experience an SUD in their lives will also experience a mental health disorder, and vice versa (1,2).
As part of our care model at YourPath, we are assessing every patient using evidence-based screeners to detect the most common co-occurring disorders. Aside from the fact such assessments should be the industry standard, we were also curious if the data we’re collecting matches what is seen in other studies.
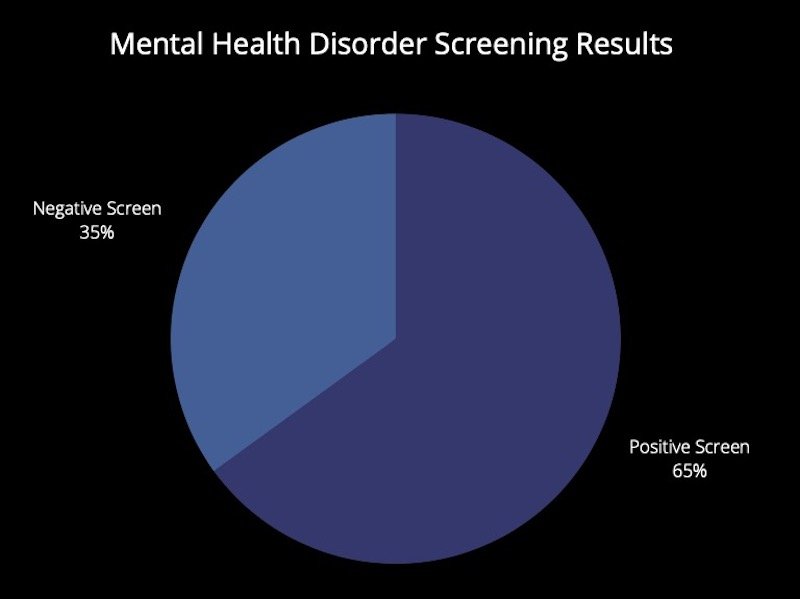
Our data show that 65% of clients who come to us for an SUD assessment screen positive for some type of mental health disorder.
Here is the breakdown of the particular mental health diagnoses that our clients screened positive for:
For better or for worse, all of the above was not particularly surprising to us. What was surprising, however, was the percentage of our clients who screened positive for a mental health disorder and are NOT receiving care.
65%!
In other words, over half of the clients who came to us for a traditional substance use disorder assessment screened positive for a mental health disorder. Of those clients, nearly 65% were not receiving care for mental health.
Why is this so important?
Individuals with co-occurring disorders exhibit significantly poorer outcomes compared with those without a mental health diagnosis, ranging from poorer treatment adherence, higher dropout rates and increased mortality (3). All of this underscores the need for integrated treatment. For far too long, mental health and SUD treatment have been siloed from each other, resulting in fragmented, inefficient and, at worst, negligent care. Additionally, the complex nature of co-occurring disorders requires specific, targeted and individualized treatment modalities, rather than the traditional one-size-fits all approach (4).
Our one goal at YourPath is to improve outcomes for everyone. Simply put, this means understanding the complexity of each individual, both at baseline and longitudinally, and embedding them within an open care network that will be compassionate and responsive to their needs. Although we are of course dismayed by the above data, we feel confident that by identifying such crucial gaps in care we have an opportunity to align the needs of the patient, family, providers and payers in a way that not only improves outcomes, but that incentives the entire system to improve outcomes.
References
Ross S, Peselow E. Co-occurring psychotic and addictive disorders: neurobiology and diagnosis. Clin Neuropharmacol. 2012;35(5):235-243. doi:10.1097/WNF.0b013e318261e193.
Kelly TM, Daley DC. Integrated Treatment of Substance Use and Psychiatric Disorders. Soc Work Public Health. 2013;28(0):388-406. doi:10.1080/19371918.2013.774673.
Kelly TM, Daley DC. Integrated Treatment of Substance Use and Psychiatric Disorders. Soc Work Public Health. 2013;28(0):388-406. doi:10.1080/19371918.2013.774673.
Mueser KT, Gingerich S. Treatment of co-occurring psychotic and substance use disorders. Soc Work Public Health. 2013;28(3-4):424-439. doi:10.1080/19371918.2013.774676.